An unknown number of Alaskans are expected to lose Medicaid coverage during the coming months as the state this week restarted an annual eligibility review that’s been on hold for three years due to the COVID-19 pandemic.
About one in three residents are currently enrolled in Medicaid, meaning officials need to do more than 260,000 reviews by March 31, 2024, according to Deb Etheridge, director of the state Division of Public Assistance. The federally mandated review started April 1, but she said no residents will have their coverage involuntarily terminated before June 1 — and even then officials are starting with relatively few reviews before speeding up the process this summer.
Also, proposals being considered by the Legislature may extend Medicaid eligibility for some residents, such as new mothers, during the coming months.
The federal government provided extra COVID-19 funding to states in exchange for keeping people enrolled in Medicaid even if their incomes rose above eligibility requirements, but the end of that provision was part of the federal budget passed in December. The public assistance division reports the current number of state enrollees is about 30,000 higher than in 2020.
“This is just reinstating that sort of traditional practice of annual renewal for our Medicaid beneficiaries,” Etheridge said during an hour-long online presentation and Q&A Tuesday hosted by the University of Alaska Anchorage.
Officials with the division and other state agencies, along with lawmakers at the Capitol, have called the year-long review an enormous undertaking and challenge — especially since the division is still catching up with a massive backlog of food stamp applications that started last summer. A fast-track supplemental budget approved by the Alaska State Legislature and signed by Gov. Mike Dunleavy at the end of March will fund 30 additional employees to help the division with the backlog and Medicaid reviews.
While other public assistance programs have also been delayed to a lesser extent due to the food stamp crisis, “there’s no redeterminations for Medicaid in the backlog,” Etheridge said.
As for how many residents are expected to lose Medicaid eligibility, she said that unlike some other states that kept separate track of people who wouldn’t be covered without the federal protections, “we did not do that here in Alaska.”
“We just continued benefits,” she said. “And so it’s very difficult for us to estimate how many individuals would remain eligible, or who may be transferred or need to go to (the Federally Facilitated Marketplace) for insurance.”
The pace is expected to start slowly with 11,000 reviews during the first months, more than 20,000 in June and continuing to increase until about 27,000 are reviewed during each of the final seven months.
“The reason that we’re kind of doing a slow ramp up is one we want to make sure that we are adequately staffed to do this, and we understand the volume and the work that needs to happen,” Etheridge said.
The first 11,000 renewal packets should reach people by April 15, after which they’ll have 45 days to submit their forms, Etheridge said.
“We won’t see any terminations until June 1” due to the state’s review process, she said. But residents could lose coverage before that date for other reasons — notably reporting a change that affects their eligibility, such as an increase in income.
The division is emphasizing people should ensure their contact information is correct, and update it if necessary online via the division’s website or by calling the state’s Medicaid Information Update Hotline (833) 441-1870.
“For some people it’s been three years since we’ve gotten any updated contact information,” Etheridge said.
Etheridge said the division is also making extra efforts to track people, including connecting to the national change-of-address database.
“I want to make sure everyone knows is that if we don’t receive the renewal package we will be doing outreach to those individuals,” she said. “We’re not just going to close individuals because we haven’t received any renewal package back.”
People losing coverage will receive a notice at least 10 days before the effective date and will be able to appeal the decision, Etheridge said.
Renewal reviews will generally occur around the anniversary of when a person’s coverage began, according to the division’s FAQ page about the process. State officials are asking residents not to submit applicant or renewal requests on their own, so that the division employees can keep up with the intended timeline.
Adding while subtracting
In addition to the fast-track money for extra public assistance employees, two bills introduced by Dunleavy would expand Medicaid eligibility for residents receiving and providing services.
One bill (House Bill 59 and its companion Senate Bill 58) extends Medicaid eligibility for new mothers to one year after giving birth instead of 60 days. The Senate version has made it through the committee process and is awaiting a floor vote, while the House version is scheduled to be heard Wednesday by the Finance Committee, its last stop before a floor vote.
A legislative fiscal analysis shows the change will cost about $2.6 million a year, with 1,596 women receiving an additional 10 months of coverage at a cost of $566.48 per month.
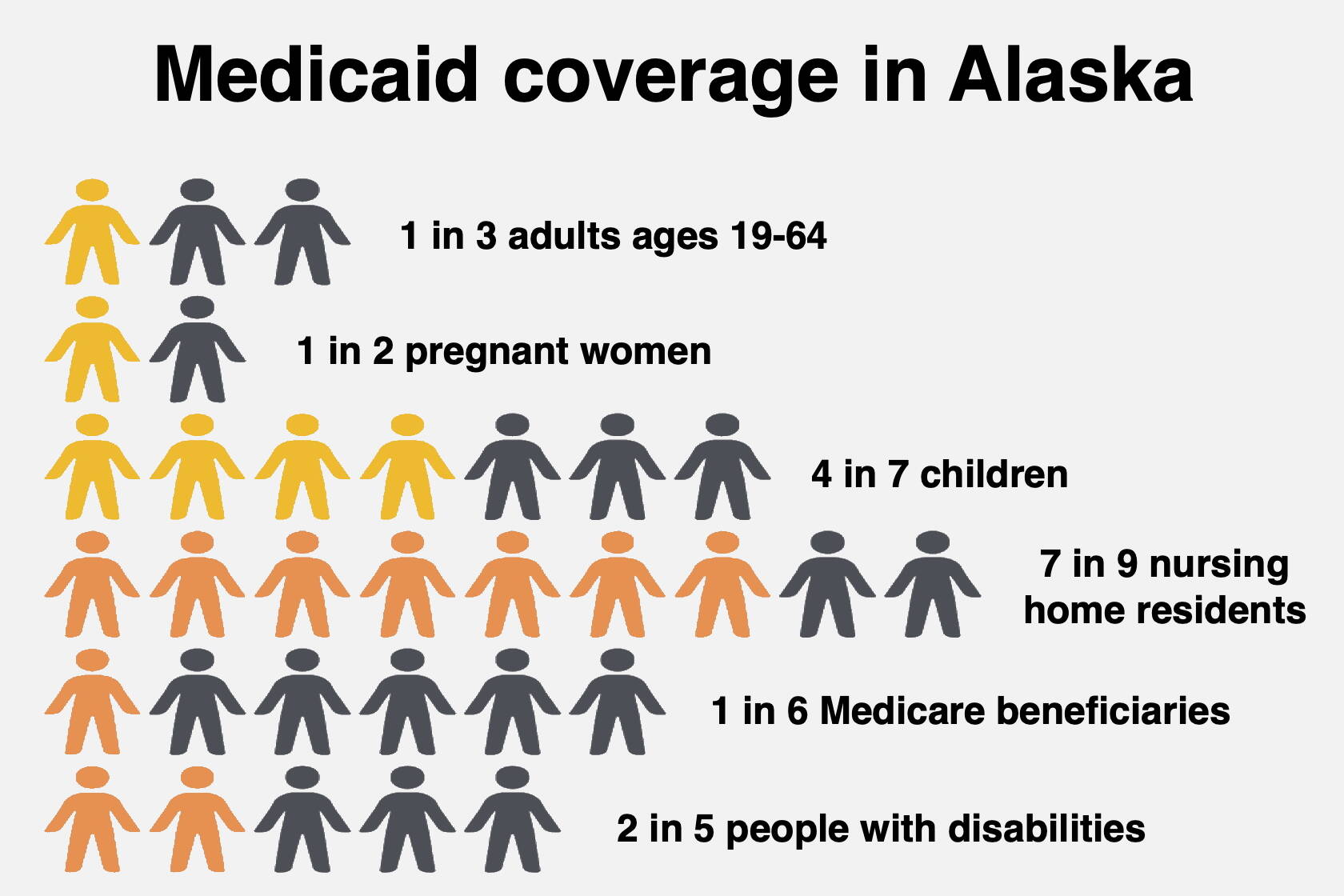
While about one-third of Alaskans were enrolled in Medicaid in 2022, the rate was about half of pregnant women and four in seven children, according to state and federal data.
Even higher were nursing home residents, with about seven in nine enrolled. They’re part of the focus of Dunleavy’s other bill (HB 58 and SB 57), which would allow people caring for an elderly adult or an adult foster child to license their home as an adult daycare, allowing them to receive Medicaid payments.
That bill is also scheduled to be heard by the House Finance Committee on Wednesday, while the Senate version is awaiting further Finance Committee action following an initial hearing in late March.
The cost of administering the program is expected to be about $270,000 a year, according to legislative fiscal reports.
Total state Medicaid funding has remained relatively stable during the past decade at roughly $600 million annually, but federal funding has increased from about $800 million in 2012 to more than $1.8 billion in 2022 as the number of enrollees has increased. Total Medicaid funding is expected to increase from about $2.4 billion in 2022 to more than $5 billion by 2042.
About 77% of Alaska’s current Medicaid spending is for people diagnosed with one or more chronic conditions, which is expected to increase to 82% by 2043. A report published by state health officials asserts efforts to reduce certain chronic conditions such as obesity, mental health, and drug and alcohol use “could lead to substantial savings” to the Medicaid program.
• Contact reporter Mark Sabbatini at mark.sabbatini@juneauempire.com